In short, no. The contraceptive patch is not suitable for everyone. While it offers a convenient weekly alternative to a daily pill, its use is strictly limited by a number of key health factors. Its safety and effectiveness are highly dependent on your weight, smoking habits, and specific medical history, particularly concerning cardiovascular risk.
The central takeaway is that the patch is a highly effective contraceptive method for the right person, but it carries significant health risks for those with specific contraindications. The decision to use it requires a careful and honest assessment of your personal health profile.

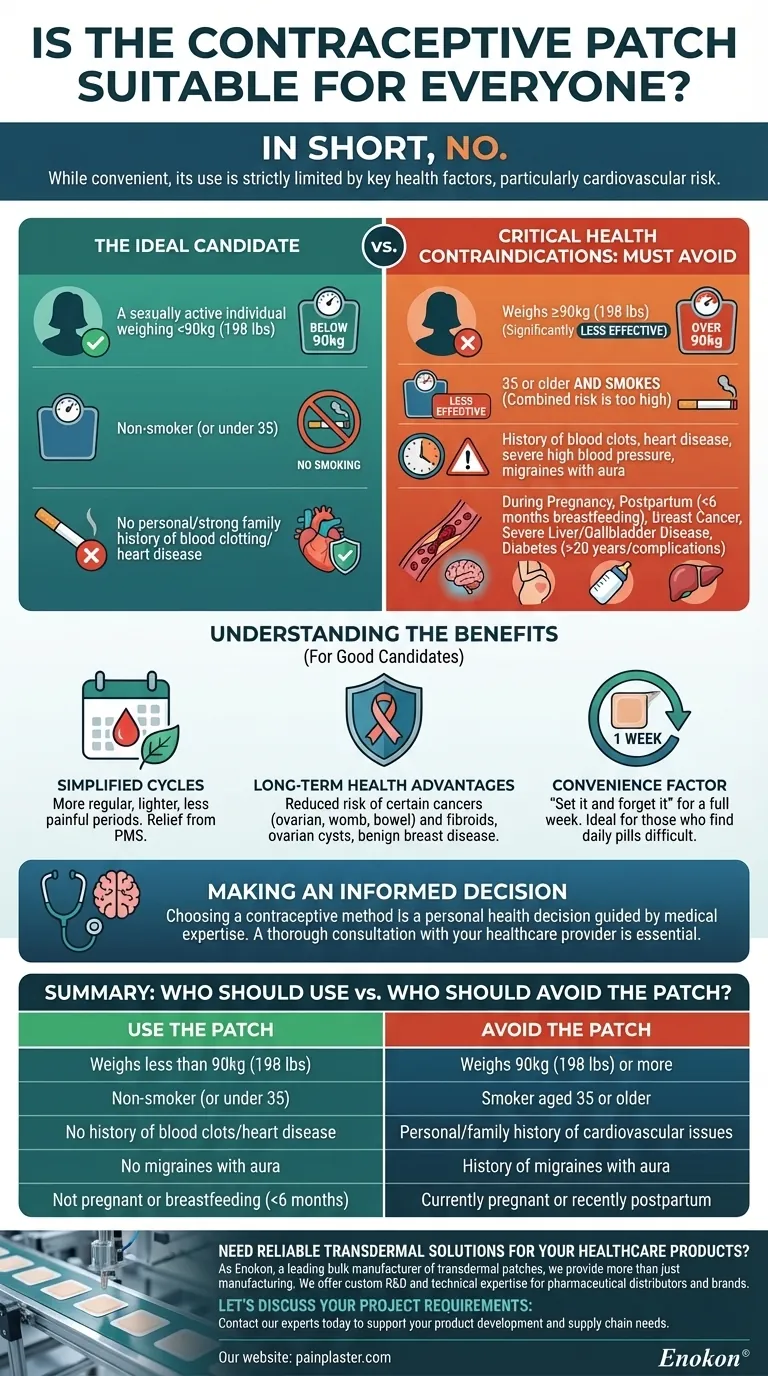
The Ideal Candidate for the Patch
For many, the patch represents a significant improvement in convenience over other methods. Its primary appeal lies in its "set it and forget it" nature for a full week at a time.
The Convenience Factor
The patch is designed for those who find a daily pill difficult to remember or who have trouble swallowing pills. You apply one patch and wear it for seven days, repeating this for three consecutive weeks, followed by one patch-free week.
The Right Health Profile
The ideal candidate is a sexually active individual who weighs less than 90kg (198 lbs). They are typically a non-smoker (or under 35) and have no personal or strong family history of blood clotting disorders or cardiovascular disease.
Critical Health Contraindications: Who Must Avoid the Patch
The hormones in the patch (estrogen and progestin) are absorbed through the skin into the bloodstream. This mechanism is why certain pre-existing conditions create unacceptable risks.
The Link Between Hormones and Blood Clots
Like many combined hormonal contraceptives, the patch can increase the risk of developing blood clots (thrombosis). This is the underlying reason for most of the restrictions on its use.
Cardiovascular and Clotting Risks
You should not use the patch if you have a personal history of blood clots, heart disease, or other circulatory diseases like severe high blood pressure. A strong family history of these conditions, especially in a relative under 45, is also a major red flag.
Age and Smoking: A Non-Negotiable Combination
This is one of the most critical contraindications. If you are 35 or older and you smoke, you cannot use the patch. This also applies if you are 35 or older and stopped smoking less than a year ago. The combined risk is simply too high.
Body Weight and Efficacy
The patch is significantly less effective in women who weigh 90kg (198 lbs) or more. For this reason, it is generally not prescribed to individuals at or above this weight.
Other Pre-existing Conditions
The patch is unsuitable if you have a history of certain medical issues. These include migraines with aura, breast cancer, severe liver or gallbladder disease, or diabetes with complications (or that you've had for more than 20 years).
During Pregnancy and Postpartum
You cannot use the patch if you are or might be pregnant. It is also not recommended for those who are exclusively breastfeeding an infant that is less than six months old.
Understanding the Benefits
For those who are good candidates, the patch offers several advantages beyond simple contraception. These benefits are a key reason why it remains a popular choice.
Simplified Menstrual Cycles
Many users experience more regular, lighter, and less painful periods. The patch can also provide significant relief from premenstrual symptoms (PMS).
Long-Term Health Advantages
Consistent use has been shown to reduce the long-term risk of developing certain types of cancer, including ovarian, womb, and bowel cancer. It can also lower your risk for fibroids, ovarian cysts, and non-cancerous breast disease.
Making an Informed Decision
Choosing a contraceptive method is a personal health decision that must be guided by medical expertise.
- If your primary focus is convenience and you fit the ideal health profile: The patch can be an excellent, low-maintenance, and effective option for you.
- If you have any history of cardiovascular issues, migraines with aura, or are over 35 and smoke: The patch is not a safe choice, and you must explore non-hormonal or different hormonal methods with your doctor.
- If you weigh 90kg (198 lbs) or more: The patch's effectiveness is compromised, and you should seek a more reliable contraceptive method.
Ultimately, a thorough consultation with your healthcare provider is the only way to confirm if the patch aligns with your individual health needs and goals.
Summary Table:
| Who Should Use the Patch? | Who Should Avoid the Patch? |
|---|---|
| Weighs less than 90kg (198 lbs) | Weighs 90kg (198 lbs) or more |
| Non-smoker (or under 35) | Smoker aged 35 or older |
| No history of blood clots/heart disease | Personal/family history of cardiovascular issues |
| No migraines with aura | History of migraines with aura |
| Not pregnant or breastfeeding (<6 months) | Currently pregnant or recently postpartum |
Need reliable transdermal solutions for your healthcare products?
As Enokon, a leading bulk manufacturer of transdermal patches and pain plasters, we provide more than just manufacturing. We offer custom R&D and technical expertise to help pharmaceutical distributors and brands develop safe, effective, and innovative transdermal delivery systems.
Let's discuss your project requirements: Contact our experts today to explore how our capabilities can support your product development and supply chain needs.
Visual Guide
Related Products
- Prostate Pain Kidney Health Care Patch for Men
- Capsaicin Chili Medicated Pain Relief Patches
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Lidocaine Hydrogel Pain Relief Patch for Pain Relief
- Icy Hot Menthol Medicine Pain Relief Patch
People Also Ask
- What lifestyle factors should be considered when choosing between testosterone patches and injections? Find Your Best Fit
- What is the purpose of testosterone patches? A Steady Solution for Low Testosterone
- What should be done before undergoing an MRI while using testosterone patches? Remove it to prevent serious burns.
- What should be done if a dose of testosterone patches is missed? Regain Stability and Safety
- What should be done if a testosterone patch is missed or falls off? Follow these simple timing rules for safety and consistency.















