The Adhesive Matrix acts as the functional heart of a transdermal drug delivery patch, serving a dual purpose that is critical to the device's success. It functions simultaneously as the primary carrier (reservoir) for the active pharmaceutical ingredient (API) and as the structural interface that bonds the device to the patient's skin. By securing a tight, uniform seal, the matrix allows drug molecules to penetrate the stratum corneum, bypass hepatic first-pass metabolism, and directly enter capillary circulation.
Core Takeaway: The Adhesive Matrix is not merely glue; it is a sophisticated delivery system that regulates drug stability and diffusion rates. Its primary goal is to maintain a consistent concentration of medication in the bloodstream by ensuring a continuous, uniform release over a specified duration (typically up to 24 hours).
The Mechanics of Drug Delivery
Acting as the Primary Drug Reservoir
In the structural design of matrix-type patches, the adhesive layer is where the active ingredients reside. The drug is dissolved or dispersed uniformly throughout this polymer structure.
This uniformity is essential. It ensures that every square centimeter of the patch contains a predictable amount of medication, allowing for accurate dosing based on the surface area in contact with the skin.
Bypassing First-Pass Metabolism
One of the most significant advantages of the adhesive matrix design is its ability to route drugs directly into the systemic circulation.
By facilitating penetration through the skin and into the capillaries, the matrix allows the drug to avoid the liver's "first-pass" metabolism. This preserves the integrity of drugs that might otherwise be broken down by the digestive system, ensuring a higher percentage of the drug actually reaches its target.
Controlling Release Kinetics
The matrix does more than hold the drug; it governs how fast the drug leaves the patch. Functional groups within the adhesive (such as those in acrylate-based or silicone adhesives) interact with the drug molecules via intermolecular forces.
These interactions control the diffusion rate, ensuring the drug is released continuously rather than in a sudden burst. This maintains steady-state plasma concentrations, preventing the dangerous peaks and ineffective valleys often seen with oral medication.
Structural and Functional Requirements
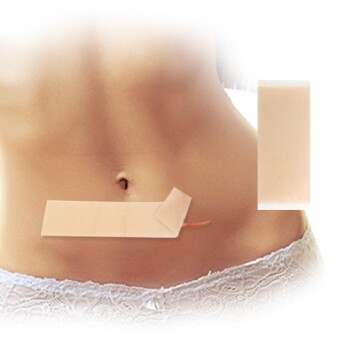
Ensuring Constant Contact Area
For a transdermal patch to work, the effective area of penetration must remain constant. If the patch lifts at the edges, the dosage drops immediately.
The Pressure-Sensitive Adhesive (PSA) within the matrix creates an immediate bond upon application. It must possess sufficient mechanical strength to remain securely attached during daily activities, ensuring the "dosage window" remains fully open for the entire application period.
Optimizing Biocompatibility
Because the matrix sits directly against the skin for extended periods (up to 24 hours), the chemical composition is critical for patient compliance.
Materials like silicone-based PSAs are often favored for their biocompatibility and breathability. A high-quality matrix minimizes skin irritation and allows moisture vapor transmission, preventing the skin underneath from becoming macerated or damaged.
Understanding the Trade-offs
Adhesion vs. Irritation
There is an inherent tension between keeping the patch on and taking it off. A matrix with aggressive adhesion ensures consistent drug delivery but risks damaging the stratum corneum upon removal.
Conversely, a gentler adhesive reduces irritation but may fail to maintain the tight contact required for effective drug permeation. The formulation must strike a precise balance: strong enough to hold, but easy to remove without leaving residue or causing trauma.
Chemical Compatibility Limitations
The adhesive matrix is chemically active. The polymer chosen must be compatible with the specific drug being delivered.
If the adhesive and the drug are chemically incompatible, it can lead to crystallization of the drug (rendering it ineffective) or degradation of the adhesive's tackiness. This requires rigorous testing to ensure the functional groups in the adhesive do not impair the drug's stability or skin permeability.
Making the Right Choice for Your Goal
Selecting the correct adhesive matrix formulation depends heavily on the specific therapeutic requirements of your drug product.
- If your primary focus is consistent therapeutic efficacy: Prioritize a matrix with precise diffusion control and strong intermolecular forces to maintain steady-state plasma concentrations without fluctuation.
- If your primary focus is patient compliance and comfort: Prioritize silicone-based matrices that offer high breathability and biocompatibility to minimize skin irritation during long-term wear.
The success of a transdermal patch ultimately relies on the Adhesive Matrix's ability to balance secure physical adhesion with precise chemical release.
Summary Table:
| Feature | Primary Function | Key Benefit to Patient |
|---|---|---|
| Drug Reservoir | Stores and stabilizes the API | Ensures accurate, uniform dosing |
| Release Kinetics | Controls the diffusion rate | Maintains steady-state plasma levels |
| Physical Adhesion | Maintains constant skin contact | Prevents dosage drops from lifting |
| Biocompatibility | Facilitates moisture transmission | Minimizes skin irritation and trauma |
Partner with Enokon for Superior Transdermal Solutions
Are you looking to develop or source high-performance transdermal drug delivery systems? Enokon is your trusted manufacturer for premium wholesale transdermal patches and custom R&D solutions.
We specialize in advanced adhesive matrix technology for a wide range of applications, including Lidocaine, Menthol, Capsicum, Herbal, and Far Infrared pain relief, as well as Eye Protection, Detox, and Medical Cooling Gel patches. Please note that our expertise covers comprehensive transdermal solutions excluding microneedle technology.
Why choose Enokon?
- Expert R&D: Custom formulations tailored to your specific API requirements.
- Proven Stability: Matrices designed for optimal drug release and chemical compatibility.
- B2B Excellence: Scalable manufacturing for global distributors and brands.
Ready to enhance your product efficacy and patient compliance? Contact us today to discuss your custom project!
References
- Begüm Ünlü, Ümit Türsen. Transdermal patches in dermatology. DOI: 10.1111/dth.12925
This article is also based on technical information from Enokon Knowledge Base .
Related Products
- Lidocaine Hydrogel Pain Relief Patch for Pain Relief
- Icy Hot Menthol Medicine Pain Relief Patch
- Menthol Gel Pain Relief Patch
- Medical Cooling Gel Patches for Fever Cooling Patches
- Far Infrared Heat Pain Relief Patches Transdermal Patches
People Also Ask
- What are the general safety guidelines for using lidocaine patches? Ensure Safe & Effective Pain Relief
- What precautions should be taken when using lidocaine patches? Essential Safety Guidelines for Proper Use
- How should lidocaine patches be applied for optimal use? Maximize Pain Relief with Proper Application
- What precautions should be taken when disposing of lidocaine patches? Protect Your Household from Accidental Poisoning
- What are common side effects of lidocaine patches? Key Risks & Safety Tips