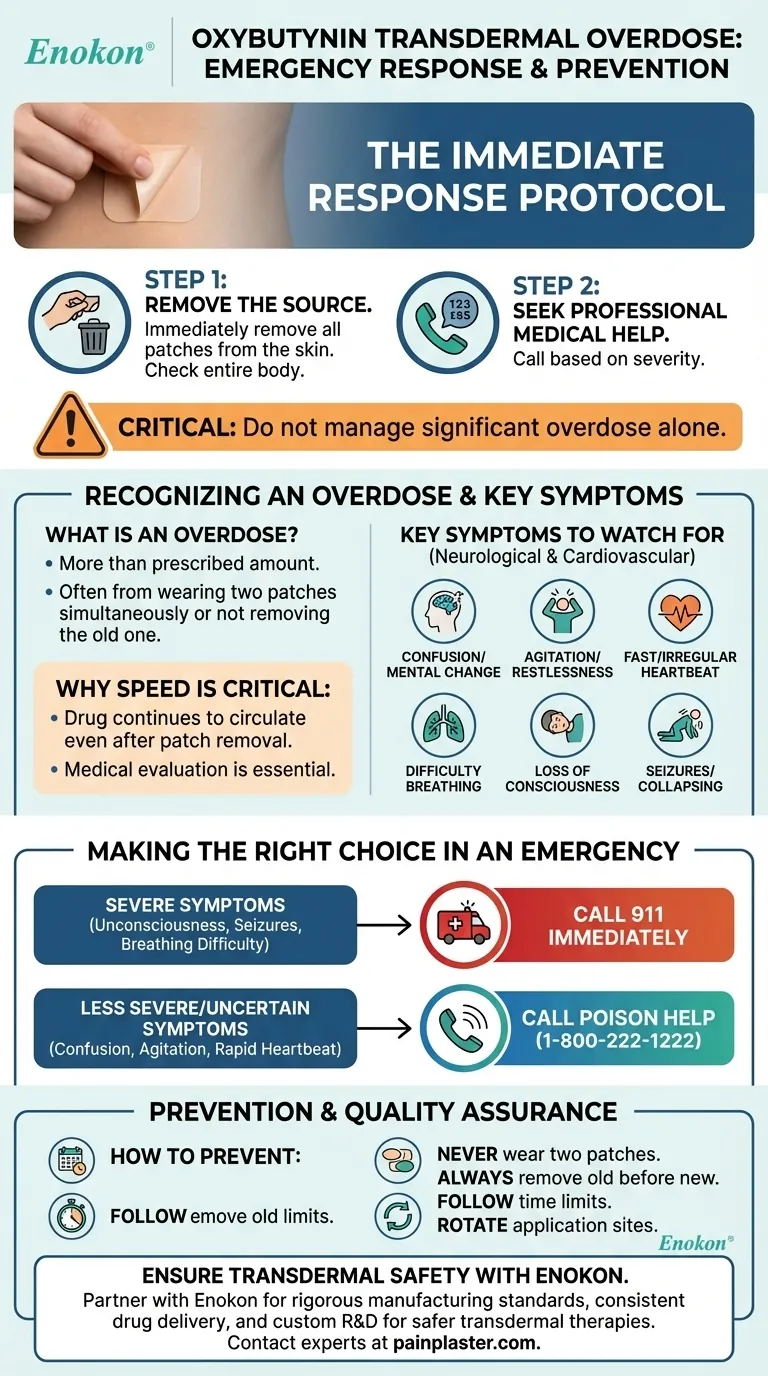
In the event of an oxybutynin transdermal patch overdose, your first action should be to remove the patch from the skin. Immediately afterward, you must seek professional medical help by either calling emergency services (911) for severe symptoms or the Poison Help line for guidance.
An oxybutynin overdose is a serious medical event that requires a two-step emergency response: remove the source of the drug and immediately contact medical professionals. Never attempt to manage significant overdose symptoms on your own.

Recognizing the Signs of an Overdose
Understanding what constitutes an overdose and its distinct symptoms is the first step toward a safe and rapid response.
What Constitutes an Overdose?
An overdose typically occurs when more than the prescribed amount of the medication is used. With transdermal patches, this most commonly happens by applying a new patch without removing the old one or wearing two or more patches simultaneously.
Key Symptoms to Watch For
The signs of an oxybutynin overdose are primarily neurological and cardiovascular. Be vigilant for the following symptoms:
- Confusion or significant changes in mental state
- Agitation and restlessness
- A fast or irregular heartbeat
- Difficulty breathing
- Loss of consciousness or inability to be awakened
- Seizures or collapsing
The presence of any of these, particularly severe symptoms like breathing trouble or loss of consciousness, signals a critical emergency.
The Immediate Response Protocol
If you suspect an overdose has occurred, follow these steps precisely and without delay.
Step 1: Remove the Source
Your first physical action should be to remove any and all oxybutynin patches from the person's body. The skin should be checked carefully, as patches can sometimes be placed in less obvious locations.
Step 2: Seek Professional Medical Help
After removing the patch, your next step depends on the victim's condition.
- For severe symptoms (unconsciousness, seizures, trouble breathing), call 911 immediately.
- For less severe symptoms (confusion, agitation), or if you are unsure, call the Poison Help line at 1-800-222-1222. Their experts will provide immediate, specific instructions.
Why Speed is Critical
A transdermal patch delivers medication steadily through the skin. Even after a patch is removed, the drug that has already been absorbed will continue to circulate in the body. This makes professional medical evaluation essential to manage the effects.
Understanding the Risks and Prevention
Proper use is the most effective way to prevent an accidental overdose and its associated dangers.
How to Prevent an Accidental Overdose
Adhering to the prescribed regimen is crucial for safety.
- Never wear two patches at once. Always remove the old patch before applying a new one.
- Follow application time limits. If you apply a patch later than usual, adjust the wearing time accordingly and do not wear it for longer than the prescribed duration.
- Rotate application sites. Consistent site rotation helps maintain healthy skin and ensures proper medication absorption, reducing the temptation to use more than one patch if irritation occurs.
Conditions That May Increase Risk
Certain pre-existing health conditions can make a person more sensitive to the effects of oxybutynin, increasing the risk of adverse reactions. These include bladder outflow obstruction, GERD, myasthenia gravis, dementia, and Parkinson's disease.
Making the Right Choice in an Emergency
Your response should be dictated by the severity of the symptoms you observe.
- If the person is unconscious, having a seizure, or struggling to breathe: Immediately call 911 for emergency services and then remove any patches if it is safe to do so.
- If the person is conscious but showing signs of confusion or a rapid heartbeat: Remove all patches from their skin and call the Poison Help line at 1-800-222-1222 for expert guidance.
- If you realize too many patches were applied but symptoms are not yet present: Remove the extra patches immediately and call the Poison Help line for preventative advice and what to monitor for.
Acting quickly and seeking professional medical advice is the most reliable way to ensure a safe outcome.
Summary Table:
| Action | Key Steps | Contact |
|---|---|---|
| Step 1: Remove Source | Immediately remove all patches from the skin. | |
| Step 2: Get Help | Severe Symptoms (unconsciousness, seizures): Call 911. Other Symptoms/Uncertain: Call Poison Help (1-800-222-1222). |
911 or 1-800-222-1222 |
| Key Overdose Symptoms | Confusion, agitation, fast/irregular heartbeat, breathing difficulty, loss of consciousness. |
Ensure the Safety and Reliability of Your Transdermal Patch Supply
An overdose incident underscores the critical importance of product quality, clear patient instructions, and reliable manufacturing. Partner with Enokon, a trusted bulk manufacturer of transdermal patches and pain plasters for healthcare and pharmaceutical distributors and brands.
We combine rigorous manufacturing standards with deep technical expertise to deliver patches with consistent drug delivery profiles, enhancing patient safety. Our team offers comprehensive custom R&D and development services to create solutions tailored to your specific drug and market needs.
Let's collaborate to develop safer, more effective transdermal therapies. Contact our experts today to discuss your requirements.
Visual Guide
Related Products
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Asthma Cough and Pain Relief Patch for Adults and Kids
- Heating Pain Relief Patches for Menstrual Cramps
- Capsaicin Chili Medicated Pain Relief Patches
People Also Ask
- What did the UK Million Women Study find regarding transdermal versus oral hormone therapy? A Safer Choice for Gallbladder Health
- Can heat patches be used for fresh injuries? Avoid This Common Mistake for Faster Recovery
- How do Deep Heat Pain Relief Patches provide pain relief? Discover the Drug-Free Mechanism
- Are heat patches safe for all body parts? Key Safety Zones and No-Go Areas Explained
- How quickly does the Deep Heat Pain Relief Back Patch activate and how long does it provide warmth? Get 16-Hour Relief















