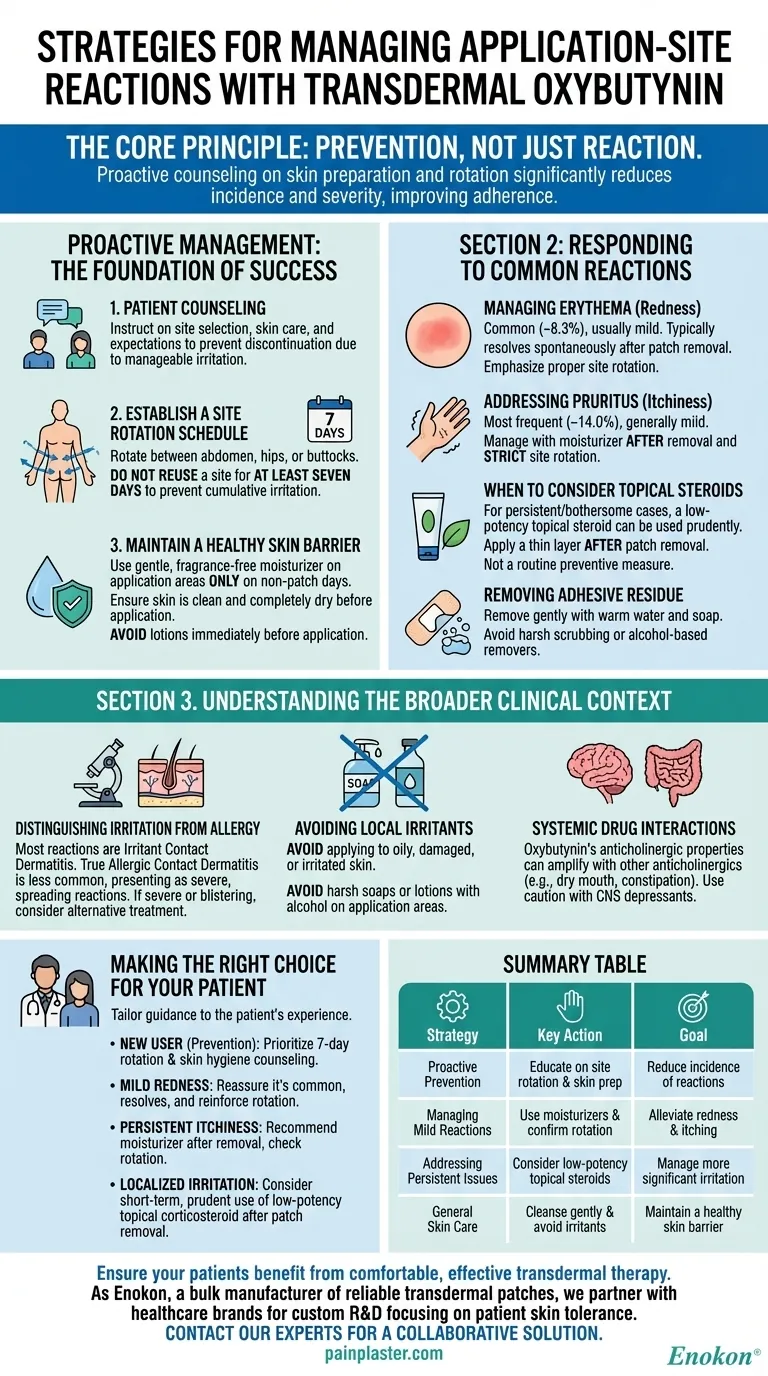
The most effective strategies for managing application-site reactions with transdermal oxybutynin are centered on proactive patient education and a systematic approach to skin care. Key interventions include establishing a consistent site rotation schedule, maintaining a healthy skin barrier, and the judicious use of topical agents like moisturizers or low-potency steroids when necessary.
The core principle is prevention, not just reaction. By counseling patients on proper skin preparation and rotation from the outset, you can significantly reduce the incidence and severity of skin reactions, thereby improving treatment adherence and overall success.

Proactive Management: The Foundation of Success
Successful long-term use of transdermal oxybutynin hinges on preparing the skin and educating the patient before problems arise. Most common reactions, such as mild erythema (redness) and pruritus (itchiness), can be minimized or avoided with the right protocol.
The Critical Role of Patient Counseling
Patient education is the single most important factor in preventing application-site issues. Clearly instruct patients on how to choose an application site, how to care for their skin, and what to expect.
This counseling significantly reduces the likelihood that a patient will discontinue therapy due to manageable skin irritation.
Establishing a Site Rotation Schedule
The skin under the patch needs time to recover. Instruct patients to establish a consistent rotation schedule for the patch, applying it to the abdomen, hips, or buttocks.
Crucially, a new application site should not be reused for at least seven days. This prevents cumulative irritation in one area.
Maintaining a Healthy Skin Barrier
Healthy, well-hydrated skin is less susceptible to irritation. Advise patients to use a gentle, fragrance-free moisturizer on the application areas, but only on days when a patch is not being worn on that specific site.
Ensure the skin is clean and completely dry before applying a new patch. Avoid using lotions or creams immediately before application, as this can interfere with adhesion.
Responding to Common Reactions
Even with proper care, mild reactions can occur. These are typically self-limiting and can be managed with simple interventions.
Managing Erythema (Redness)
Erythema is a common reaction, affecting approximately 8.3% of users. It is usually mild to moderate in severity.
This redness typically resolves spontaneously after the patch is removed and does not require specific treatment beyond proper site rotation.
Addressing Pruritus (Itchiness)
Itchiness is the most frequent reaction, reported by about 14.0% of users. It is also generally mild.
This symptom can be managed effectively by applying moisturizers to the area after the patch is removed and by strictly adhering to the site rotation schedule.
When to Consider Topical Steroids
For persistent or more bothersome itching and redness, a low-potency topical steroid may be used prudently.
Apply a thin layer to the affected area after the patch has been removed. This should be considered a secondary option, not a routine preventive measure.
Removing Adhesive Residue
Some patch adhesive may remain on the skin after removal. This residue can be a source of minor irritation.
Instruct patients to remove it gently using warm water and soap. Harsh scrubbing or alcohol-based removers should be avoided as they can irritate the skin.
Understanding the Broader Clinical Context
Managing local skin reactions is key, but it must be done within the full clinical picture of the medication and the patient.
Distinguishing Irritation from Allergy
The vast majority of reactions are irritant contact dermatitis, caused by the adhesive or the medication itself. A true allergic contact dermatitis is much less common but may present with more severe, spreading reactions.
If a reaction is severe, blistering, or extends well beyond the patch site, an alternative treatment should be considered.
Avoiding Local Irritants
Advise patients to avoid applying the patch to skin that is oily, damaged, or irritated. Furthermore, they should avoid using harsh soaps or lotions containing alcohol on the application areas.
Systemic Drug Interactions
While unrelated to skin reactions, remember that oxybutynin has systemic effects. Its anticholinergic properties can be amplified when used with other drugs in the same class, increasing side effects like dry mouth and constipation.
Use caution when co-administering with CNS depressants or any medication that can cause drowsiness.
Making the Right Choice for Your Patient
Your guidance should be tailored to the patient's experience to ensure they can continue to benefit from this effective therapy.
- If your primary focus is prevention for a new user: Prioritize detailed counseling on a strict seven-day site rotation schedule and proper skin hygiene from day one.
- If your patient is experiencing mild, intermittent redness: Reassure them that this is common and typically resolves on its own, and reinforce the importance of site rotation.
- If your patient complains of persistent itchiness: Recommend applying a quality moisturizer to the site after patch removal and confirm they are not reusing sites too frequently.
- If a patient has more significant but localized irritation: Consider the short-term, prudent use of a low-potency topical corticosteroid on the affected skin after the patch is off.
By implementing these straightforward strategies, you can empower patients to manage side effects, fostering the long-term adherence needed for successful treatment.
Summary Table:
| Strategy | Key Action | Goal |
|---|---|---|
| Proactive Prevention | Educate on site rotation & skin prep | Reduce incidence of reactions |
| Managing Mild Reactions | Use moisturizers & confirm rotation | Alleviate redness & itching |
| Addressing Persistent Issues | Consider low-potency topical steroids | Manage more significant irritation |
| General Skin Care | Cleanse gently & avoid irritants | Maintain a healthy skin barrier |
Ensure your patients benefit from comfortable, effective transdermal therapy. As Enokon, a bulk manufacturer of reliable transdermal patches and pain plasters, we partner with healthcare and pharma distributors and brands. Our technical expertise supports custom R&D and development to create patches that prioritize patient skin tolerance and adherence. Let's discuss how we can enhance your product line – contact our experts today for a collaborative solution.
Visual Guide
Related Products
- Far Infrared Heat Pain Relief Patches Transdermal Patches
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Asthma Cough and Pain Relief Patch for Adults and Kids
- Heating Pain Relief Patches for Menstrual Cramps
- Capsaicin Chili Medicated Pain Relief Patches
People Also Ask
- What are the key features of the Deep Heat Pain Relief Back Patch? Get Up to 16 Hours of Drug-Free Relief
- What are the common side effects of using the medicated heat patch? Understanding Risks & Safe Use
- How does capsaicin work in the medicated heat patch? The Science Behind Pain Relief
- How does the Deep Heat Back Patch work? A Drug-Free Solution for Targeted Pain Relief
- What types of pain can the Deep Heat Pain Relief Back Patch be used for? Targeted Relief for Muscles & Joints














