At its core, transdermal buprenorphine works by delivering a specific type of opioid through the skin to alter how your brain and nervous system respond to pain. It belongs to a class of medications called opiate analgesics, which function by partially activating the opioid receptors in your body, producing a powerful pain-relieving effect.
Buprenorphine is not a typical opioid. It functions as a "partial agonist," providing continuous, steady pain relief for severe, long-term conditions, making it fundamentally different from medications used for short-term or as-needed pain management.

The Mechanism of Action: A Closer Look
To understand how transdermal buprenorphine works, we need to look at both its chemical nature and its delivery system. Each component plays a critical role in its effectiveness.
Targeting the Opioid Receptors
Your body has a system of opioid receptors located in the brain, spinal cord, and other areas. When activated, these receptors block pain signals from being sent and reduce the perception of pain. Buprenorphine binds to these same receptors to produce its analgesic (pain-relieving) effect.
The "Partial Agonist" Difference
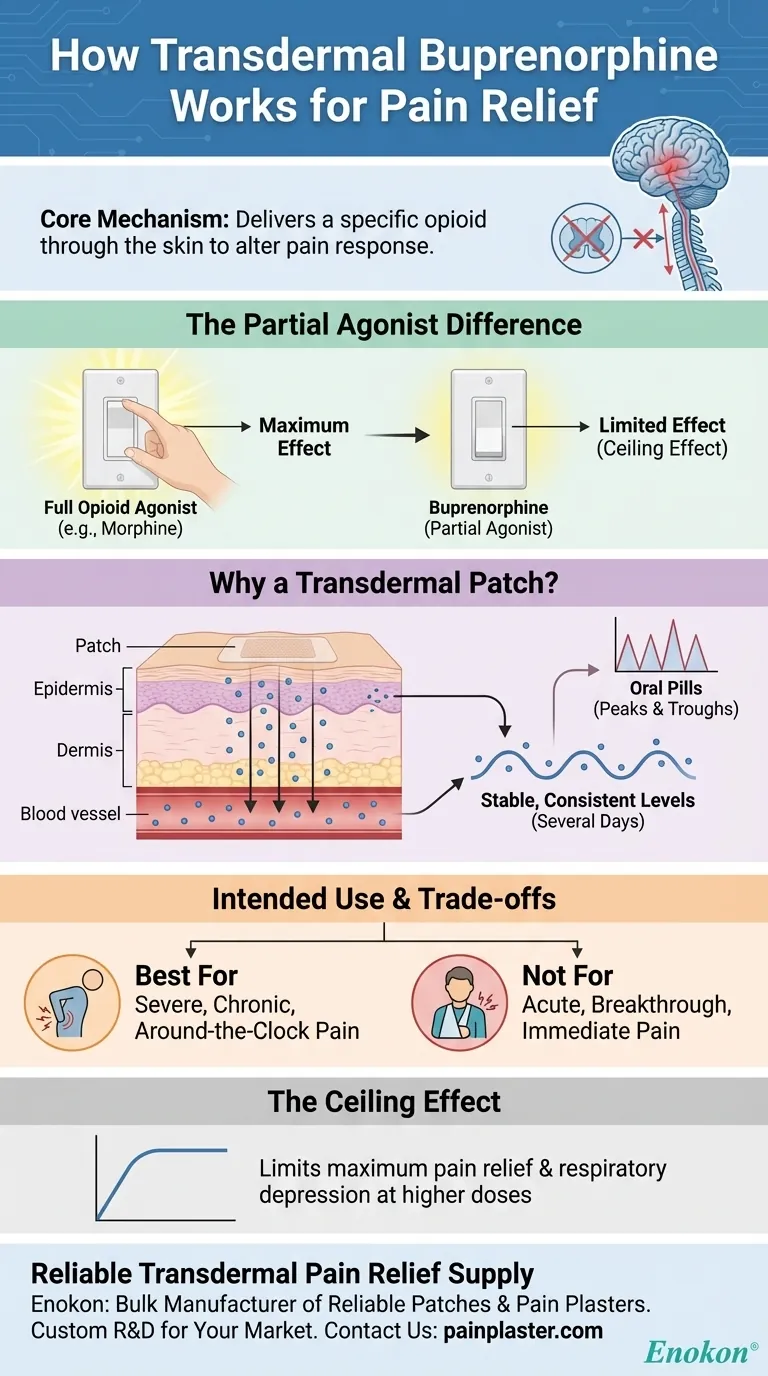
Unlike full opioid agonists like morphine or oxycodone, which activate receptors to their maximum capacity, buprenorphine is a partial agonist.
Think of an opioid receptor as a light switch with a dimmer. A full agonist turns the dimmer all the way up, producing the strongest possible effect. Buprenorphine, the partial agonist, can only turn the dimmer up part-way, providing significant pain relief but with a natural limit or "ceiling" to its effects.
Why a Transdermal Patch?
The delivery system is just as important as the drug itself. A transdermal patch provides a unique advantage for managing a specific type of pain.
The patch allows the medication to be absorbed slowly and continuously through the skin into the bloodstream. This creates stable, consistent levels of the drug in your body over several days, avoiding the peaks and troughs associated with oral pills. This steady state is ideal for managing constant, around-the-clock pain.
Understanding the Trade-offs and Intended Use
Buprenorphine's unique properties make it a highly specialized tool, not a general-purpose pain reliever. Understanding its limitations is crucial for its safe and effective use.
Intended for Severe, Chronic Pain Only
The buprenorphine patch is specifically designed for severe and persistent pain that requires continuous, long-term opioid treatment. It is not intended for mild pain, short-term pain (like after a surgery), or pain that can be managed with as-needed medication.
The Ceiling Effect
The partial agonist nature of buprenorphine creates a "ceiling effect." This means that beyond a certain dose, taking more of the medication does not produce a stronger pain-relieving effect. This can also limit its respiratory depression effects, which is a potential safety benefit, but it also means it may not be sufficient for the most extreme pain scenarios.
Not for Immediate Relief
Because the medication is absorbed slowly through the skin, it takes a significant amount of time to reach effective levels in the bloodstream. The patch is not suitable for acute or "breakthrough" pain that requires immediate relief.
Making the Right Choice for Your Pain
Understanding these principles helps clarify when this medication is the appropriate choice.
- If your primary focus is managing persistent, around-the-clock pain: The patch's steady, continuous delivery system is designed specifically for this purpose.
- If your primary focus is treating short-term or breakthrough pain: This medication is inappropriate due to its slow onset and long-acting nature.
- If you have experienced significant side effects with full opioid agonists: The unique partial agonist action of buprenorphine may offer a different risk-benefit profile under medical supervision.
Ultimately, the use of transdermal buprenorphine is a strategic decision for managing a very specific type of pain.
Summary Table:
| Key Aspect | How Transdermal Buprenorphine Works |
|---|---|
| Mechanism | Acts as a partial agonist on opioid receptors in the brain and spinal cord. |
| Delivery | Slow, continuous absorption through the skin for stable drug levels. |
| Key Benefit | Provides around-the-clock relief for severe, chronic pain. |
| Ceiling Effect | Limits maximum effect and certain side effects at higher doses. |
| Best For | Managing persistent, long-term pain, not immediate or breakthrough pain. |
Need a reliable supply of transdermal pain relief patches?
As Enokon, a bulk manufacturer of reliable transdermal patches and pain plasters, we provide healthcare and pharmaceutical distributors and brands with high-quality products backed by technical expertise. Benefit from our custom R&D and development services to create the perfect pain management solution for your market.
Contact our team today to discuss your requirements and how we can support your product development.
Visual Guide
Related Products
- Lidocaine Hydrogel Pain Relief Patch for Pain Relief
- Far Infrared Deep Heat Relief Patches Medicated Pain Relief Patches
- Far Infrared Knee Pain Patch Heat Patches for Pain Relief
- Far Infrared Pain Patch Relief Pain Reliever for Back
- Far Infrared Heat Pain Relief Patches Transdermal Patches
People Also Ask
- Are lidocaine patches safe to use during pregnancy? A Guide to Making an Informed Choice
- Is it safe to use lidocaine patches while breastfeeding? Expert Guidance for Nursing Mothers
- How should the treated area be protected while wearing a lidocaine patch? Safety Tips for Effective Pain Relief
- How can you use lidocaine patches for multiple sore spots? A Guide to Safe, Effective Pain Relief
- What systemic side effects can lidocaine patches cause? Minimizing Risks for Safe Pain Relief
















